Dry Eye Treatment

3-D OSA ocular surface analyzer
Intense pulsed light therapy (IPL)


The following parameters can be measured by OSA, and each parameter plays an important role in identifying the DED type

The size of the tear meniscus formed at the edges of the eyelids provides useful information on the volume of tear fluid produced. The lacrimal meniscus can be examined for its height, regularity and shape. Assessment of the amount of tear film uses magnification tools; you can measure the height of the tear meniscus and evaluate its characteristics along the lower lid margin.
Measurement of BUT by a non-invasive technique eliminates the disruption of the tear film caused by the instillation of the fluorescein dye. The stability of the mucin layer and the entire tear film is measured by NIBUT using grids projected onto the cornea. You can manually or automatically judge when the tear disintegrates.
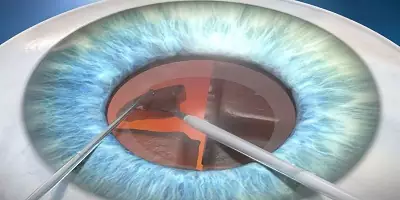
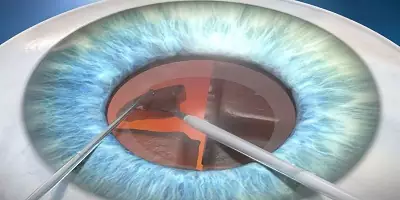
Describes the morphology of the glands to diagnose each meibomian gland. Further details fall out that would lead to lacrimal dysfunction. Meibography is the visualization of the glands by transillumination of the eyelid with infrared light. Meibomian gland dysfunction destabilizes tears, causing evaporative dry eye. The posterior lamella of the eyelid hosts a fleet of meibomian glands located between the eyelid conjunctiva and the tarsal plate. A normal meibomian gland is approximately linear and 3-4 mm long and extends across the posterior lid perpendicularly from the lid margin to the opposite tarsal margin.
This test helps detect blepharitis and demodex, which can be done on the outer surface of the eye and eyelids.
After you take the picture of the conjunctival blood vessels, you can compare them with the bulbar and limbal redness degree classification sheets.
The Advantages of IPL
- Using strong pulsed light to treat MGD cases tends to alleviate dry eye symptoms.
- The meibomian gland activity is increased, the tear film is balanced, and ocular surface inflammation is reduced after IPL therapy.
- IPL improves tear film homeostasis and alleviated ocular symptoms in cases with refractory MGD, making it a potential treatment option for this disorder.
- Meibum consistency, meibum expressibility, lid margin abnormality, ocular surface staining, tear film breakup period (TBUT), and the Ocular Surface Disease Index (OSDI) all improved significantly after IPL.
